A World Antimicrobial Resistance Week Special
As part of the World Antimicrobial Resistance Week (November 18-23) we discussed the critical issue with our expert DR AMIT DIAS from the Department of Preventive & Social Medicine, GMC. “We need to prevent anti-microbial resistance together,” cautioned Dr Dias as he elaborated on the crucial role played by everyone. Read this informative interview and contribute to the fight against anti-microbial resistance.
Goan Observer: Doctor, what is antimicrobial resistance?
Dr Dias: Antimicrobial resistance is a global health concern that occurs when bacteria, viruses and other microorganisms evolve and adapt, rendering antibiotics ineffective. The World Health Organization (WHO) has identified it as one of the greatest threats to public health. It is estimated that bacterial AMR is directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths. If we don’t address this issue, the number is expected to rise. When the microorganism develops resistance to the drug, it becomes difficult to treat and we often have to opt for more expensive and toxic medication to save the patient affected by the resistant bug.
Q: That is a major concern indeed. What is the aim of the campaign this year?
A: The World AMR Awareness Week is a global campaign to raise awareness and understanding of AMR and promote best practices among One Health stakeholders (animal husbandry, health professionals, and forest department officials) to reduce the emergence and spread of drug-resistant infections. The theme for WAAW 2023 is “Preventing antimicrobial resistance together.” AMR is a threat to humans, animals, plants and the environment and we need to fight it together.
Q: What are the reasons for the rise of antimicrobial resistance?
A: There are several factors at play here. Over-prescription and misuse of antibiotics are major contributors. When antibiotics are used unnecessarily or not as prescribed, bacteria have a higher chance of developing resistance. Additionally, the use of antibiotics in agriculture and livestock for growth promotion and disease prevention also contributes to the problem. Poor infection control practices in healthcare settings can further accelerate the development and spread of resistant strains. That’s the reason I said we need to have a collaborative effort to fight resistance.
Q: Could you elaborate on the implications of antimicrobial resistance? How does it impact patients and public health?
A: Antibiotic resistance can lead to prolonged illness, increased healthcare costs and higher mortality rates. Imagine a common infection that was once easily treatable becoming untreatable due to resistance. Procedures like surgeries and chemotherapy, which rely on the prevention and treatment of infections, become riskier. Previously manageable infections could become life-threatening. This not only affects individuals but has broader societal and economic implications.
Q: Can you provide some examples of situations where antibiotic resistance has had severe consequences?
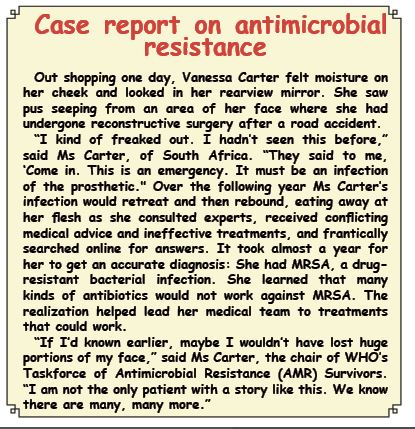
A: Certainly. One example is the rise of methicillin-resistant Staphylococcus aureus (MRSA), a bug that causes infections and is resistant to several antibiotics. Another example is the emergence of extensively drug-resistant tuberculosis (XDR-TB), where the bacteria are resistant to the most potent first-line and second-line drugs. These cases highlight the urgency of addressing antibiotic resistance to prevent further complications. Someone on anti-TB treatment must complete the whole course. If they stop midway, because they feel fine, they will give the bug a chance to develop resistance.
Q: Given the severity of the issue, what measures can individuals and communities take to prevent antibiotic resistance?
A: As the theme suggests everyone has an important role to play. First and foremost, healthcare professionals must prescribe antibiotics judiciously and for patients to take them exactly as prescribed. Public education on the proper use of antibiotics is essential. In agriculture, there should be a responsible use of antibiotics with a focus on alternatives and good hygiene practices.
Communities play a vital role in this fight. Awareness campaigns such as these can help educate the public about the consequences of antibiotic misuse. People should not self-prescribe antibiotics and should complete the prescribed course. Proper hygiene, vaccination, and infection prevention measures are also crucial in reducing the need for antibiotics in the first place.
Q: Thank you for shedding light on this critical issue. Any message for our readers?
A: Be aware of your role in preventing AMR and inform others as well. A collective effort is needed to combat AMR and preserve the effectiveness of these life-saving drugs.