Goa is abuzz with excitement as vintage bike and car owners, users, collectors and fans are decking […]
THE A to Z ON DIABETES: Diabetes education for all!By Dr Amit Dias, MD
MIND & BODY, HEART & SOUL, Nov 16- Nov 22 2024 November 15, 2024November 14 is World Diabetes Day!
This year’s theme for World Diabetes Day is “Breaking Barriers, Bridging Gaps.” It emphasizes the need to raise awareness and improve accessibility to appropriate diabetes care. Dr Amit Dias in this enlightening article explains the A to Z on diabetes. Diabetes affects millions globally, leading to serious health complications if left untreated….
Read and enlighten others – Let’s fight diabetes together
A – Awareness & Access
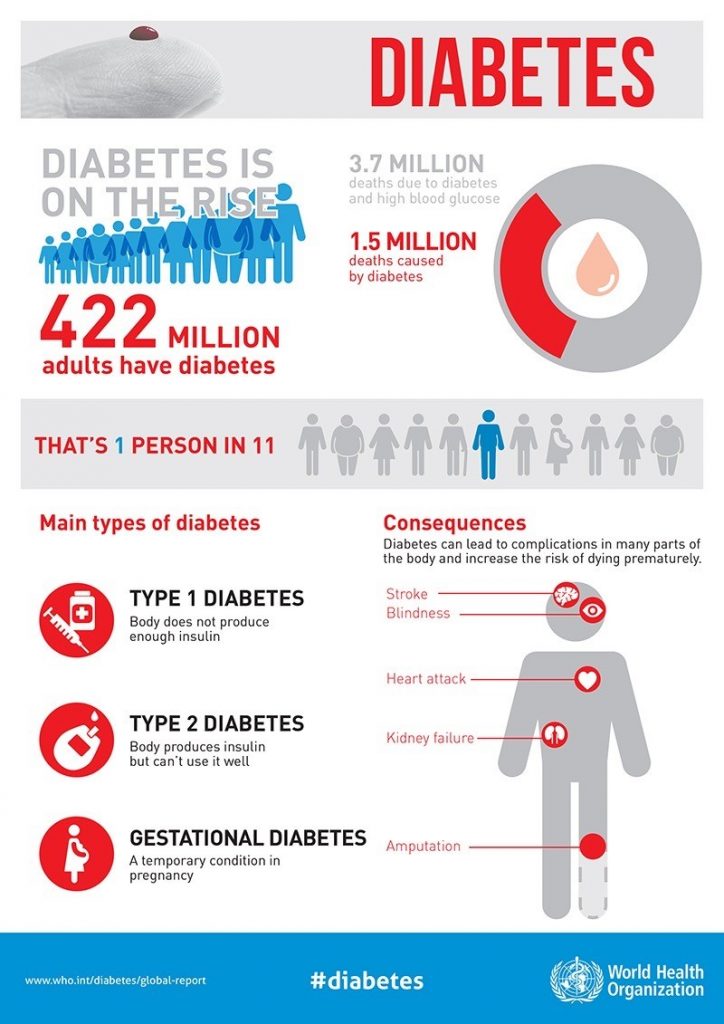
WITH an estimated 422 million adults with diabetes, awareness and access to good quality diabetes care is crucial to break barriers and build bridges in diabetes management. Early diagnosis and understanding risk factors reduce complications. Public health campaigns are essential for early diagnosis and preventive strategies, particularly for high-risk individuals.
Goa has a high prevalence of diabetes (26.4% above age 20) in the country, and is working to reverse this trend through lifestyle change and public education. There are several innovative strategies implemented by the government to bridge the gaps in diabetes care. The difference will be seen when the people avail these facilities and take control with the support of the health care system.
B – Blood Sugar Levels
Monitoring blood sugar is foundational. Key diagnostic targets from ICMR for diabetes include:
Fasting Blood Sugar: ≥126 mg/dL (diabetes); 110-125 mg/dL (prediabetes).
Post Prandial Blood Sugar: ≥200 mg/dL (diabetes); 140-199 mg/dL (prediabetes).
HbA1c: ≥6.5% (diabetes); 5.7-6.4% (prediabetes).
Random Plasma Glucose: ≥200 mg/dL with symptoms.
Self-monitoring helps manage glucose levels, reducing risks of hyper- and hypoglycemia.
C – Cholesterol
INDIVIDUALS with diabetes often face higher cardiovascular risks due to elevated LDL (bad) cholesterol and reduced HDL (good) cholesterol. Specific targets for managing lipids in people with diabetes are:
• LDL cholesterol: <100 mg/dL, or <70 mg/dL for those with existing cardiovascular disease. • HDL cholesterol: >40 mg/dL for men, >50 mg/dL for women.
• Triglycerides: <150 mg/dL
D – Diet
DIET plays a central role in managing blood sugar. The focus should be on high-fiber carbohydrates, lean proteins and healthy fats. Key dietary strategies include:
• Carbohydrate counting: Limiting carbs to around 45-60 grams per meal, depending on individual needs.
• Portion control: Helps to avoid spikes in blood sugar.
A dietitian can personalize dietary recommendations to support glycemic control. A diet rich in omega-3s, fiber and low in trans fats can help maintain healthy cholesterol levels.
E – Exercise
EXERCISE improves insulin sensitivity and aids in blood sugar control. The American Diabetes Association recommends at least:
• 150 minutes of moderate-intensity aerobic exercise weekly (for example, brisk walking).
• Strength training: At least twice a week, targeting all major muscle groups.
Exercise should be consistent, with no more than two consecutive days without physical activity, to sustain insulin sensitivity benefits.
F – Fiber
FIBER slows the digestion of carbohydrates, aiding blood sugar control. The recommended daily intake is 25–30 grams, with emphasis on:
• Soluble fiber: Found in oats, legumes, and fruits.
A high-fiber diet can also support weight management, reduce LDL cholesterol, and improve cardiovascular health.
G – Glycemic Index
THE Glycemic Index (GI) ranks carbohydrates based on their impact on blood glucose levels. For better glucose control, individuals with diabetes should focus on:
• Low-GI foods (GI <55): Most fruits, vegetables, and whole grains.
Lower-GI foods release glucose slowly, preventing post-meal spikes.
H – HbA1c
IF YOU are having diabetes and have not done your HbA1c test, then please speak to your doctor about it. HbA1c provides the average blood glucose over the past 2-3 months and is a critical marker for long-term management. The general target for HbA1c is <7% for many adults with diabetes, though targets may be individualized.
HbA1c reflects overall control and can guide therapy adjustments.
I – Insulin
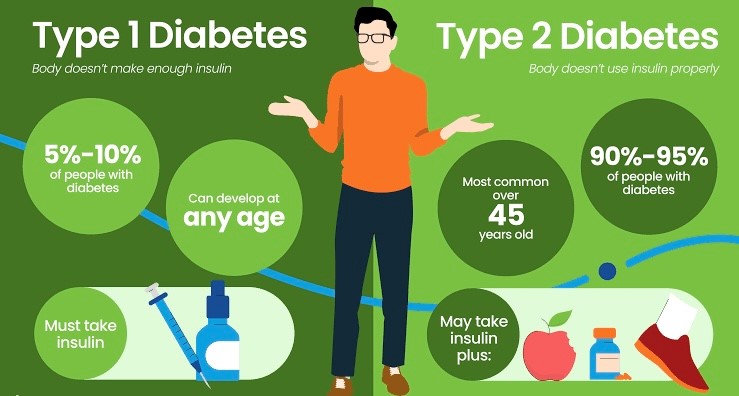
INSULIN is essential for glucose metabolism, particularly in Type 1 diabetes and some cases of Type 2 diabetes. There are various types of insulin:
• Rapid-acting: Covers meals (e.g., Lispro, Aspart).
• Long-acting: Provides baseline insulin (e.g., Glargine, Detemir).
An understanding of timing and types of insulin is critical for effective diabetes management. Do not be afraid of taking insulin, understand the technique from your treating physician and diabetes educator.
J – Journaling
JOURNALING daily food intake, blood sugar levels, physical activity and medication can help in tracking patterns and making informed decisions. Noting down blood glucose before and after meals, physical activity, and symptoms of hyper- or hypoglycemia can provide invaluable insights.
K – Ketones
HIGH ketone levels indicate the body is breaking down fat for energy, which can happen in cases of insufficient insulin, particularly in Type 1 diabetes. Testing ketones is essential when blood glucose is persistently high (>250 mg/dL) as it can indicate diabetic ketoacidosis (DKA), a life-threatening condition.
L – Lifestyle Changes
LIFESTYLE changes is the key strategy to combat the epidemic of diabetes. Sustainable lifestyle changes such as healthy eating, regular exercise, weight management, and stress reduction are extremely crucial in diabetes management. Reducing alcohol intake and quitting smoking also lower cardiovascular risks. Structured lifestyle programs have been proven to help prevent, delay and even reverse Type 2 diabetes.
M – Monitoring
FREQUENT blood glucose monitoring allows for prompt corrective actions and adjustments in diet, medications, and lifestyle. CGMs are increasingly popular, offering real-time glucose data and reducing the need for finger-pricks. Monitoring helps prevent hyper- and hypoglycemic episodes, particularly in individuals on insulin.
N – Nutrition Education
NUTRITION education empowers individuals to make informed choices about food and its impact on blood sugar. It encompasses understanding carbohydrate content, portion sizes, and reading food labels. A dietitian or your physician can provide individualized guidance, improving long-term outcomes.
O – Obesity
OBESITY is a major modifiable risk factor for Type 2 diabetes. The risk increases with:
• BMI >25 (overweight) and BMI >30 (obesity).
• Waist circumference: >40 inches in men and >35 inches in women.
Obesity causes insulin resistance, weight loss of just 5-10% can significantly improve blood glucose control and insulin sensitivity.
P – Prevention
THE good news is that unlike what we felt before, evidence shows that Type 2 diabetes can be prevented and, in some cases, reversed through lifestyle changes. Major studies, like the Diabetes Prevention Program (DPP), demonstrated that losing 5-7% of body weight and engaging in at least 150 minutes of moderate-intensity exercise per week can lower diabetes risk by 58% in high-risk individuals.
Studies reveal that a low-calorie diet can lead to remission. The DIRECT trial (Diabetes Remission Clinical Trial) found that nearly 46% of participants with Type 2 diabetes achieved remission through significant weight loss via meal replacement.
These findings underscore the potential of diet, exercise, and weight management in both preventing and, for some, reversing Type 2 diabetes, especially in its early stages.
Q – Quality of Life
PROPER glucose monitoring and prevention of complications in diabetics is essential to maintain a good quality of life. Good management also includes- stress management, balanced lifestyle practices, and regular check-ups with healthcare providers.
R – Risk Factors
THE main risk factors include age over 45, family history, obesity, sedentary lifestyle, high blood pressure, and high cholesterol levels. Indians face higher diabetes risk due to genetic predisposition, abdominal obesity (with cut-offs of 90 cm for men and 80 cm for women), and insulin resistance even at lower body weights. Diets high in refined carbs and low in fiber further elevate risk. A sedentary lifestyle, early onset (often between ages 25-45), and rapid urbanization add to this vulnerability, as physical activity decreases and high-calorie foods become more accessible. Socioeconomic transitions have accelerated these risk factors, making lifestyle interventions and regular screenings essential to managing diabetes risk among Indians.
S – Stop Smoking
SMOKING significantly increases the risk of complications in individuals with diabetes, including heart disease, stroke, and kidney disease. Nicotine affects insulin action, making blood sugar control more difficult, while smoking-related inflammation raises cardiovascular risks. Quitting smoking can improve blood circulation, enhance insulin sensitivity, and reduce the risk of nerve and kidney damage.
Smoking cessation is a critical component of diabetes management. Individuals with diabetes should be encouraged to seek support through counseling, medications, or smoking cessation programs to improve their overall health and reduce diabetes-related complications. Smoking cessation clinics have been started at the GMC and the district hospitals in Goa.
T – Types of Diabetes and Technology use
Types of Diabetes:
There are mainly three types of diabetes: Type 1 (autoimmune, insulin-dependent), Type 2 (insulin resistance-related), and Gestational (pregnancy-related). Each type requires specific management strategies.
Technology: Advancements like Continuous Glucose Monitors (CGMs), insulin pumps, and diabetes apps enhance blood glucose monitoring and insulin administration, offering personalized, real-time diabetes management and improved control.
U – Understanding Complications
DIABETES can lead to severe complications, including neuropathy, retinopathy, kidney disease, and cardiovascular issues. Regular check-ups help detect these complications early, allowing for timely interventions. Guidelines suggest annual eye exams to screen for retinopathy, foot exams for neuropathy, and urine tests for kidney health. Blood pressure and lipid profiles should be checked regularly, as diabetes increases cardiovascular risk.
The American Diabetes Association (ADA) recommends HbA1c tests at least twice a year (or more frequently if glucose levels are uncontrolled) to assess long-term blood sugar management. Following these guidelines can significantly reduce the risk of severe complications through early detection.
V – Visits to Healthcare Professionals
AS mentioned above, regular check-ups are critical for comprehensive diabetes care, including assessments of HbA1c, blood pressure, lipid levels, and kidney function. These visits allow for treatment adjustments and early intervention.
W – Weight Management
WEIGHT management is vital for reducing insulin resistance. A healthy BMI (18.5-24.9) and waist circumference below risk thresholds improve glucose control. Strategies like mindful eating, portion control, and structured exercise can support weight loss.
X – Syndrome X (Metabolic Syndrome)
SYNDROME X, also known as metabolic syndrome, includes factors like high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels. This syndrome significantly raises the risk for diabetes and cardiovascular disease. Managing each component of metabolic syndrome is essential in diabetes prevention and control.
Y – Yearly Check-ups
ANNUAL check-ups are essential to assess diabetes-related complications, including tests for microalbumin (to check kidney health), eye exams for retinopathy, and foot exams. Regular assessments help manage complications proactively.
Z – Zinc
ZINC is involved in insulin production and glucose regulation. Adequate intake is beneficial for insulin sensitivity, with sources including meat, shellfish, legumes, and whole grains. Zinc supplementation may benefit those with deficiency but should be used with caution to avoid overuse.