Goa is abuzz with excitement as vintage bike and car owners, users, collectors and fans are decking […]

PERSON-CENTERED CARE: Need of the hour for seniors
Dec 21- Dec 27 2024, MIND & BODY, HEART & SOUL December 20, 2024This week we caught up with Dr Amit Dias while he was at the newly launched Assistive Living facility for elders and people with dementia called Aaji Care. As he spoke on graceful ageing, he said “We need to promote person-centered care. We should approach the person with the disease and not the disease with the person.” In his thought provoking keynote address, he added, “Person-centered care is not only an approach in assisted living facilities, but also in the home for family caregivers.”
Q&A Interview with Dr Amit Dias
Goan Observer: Thank you for joining us, to begin with can you explain what person-centered care is all about?
Dr Amit Dias: Person-centered care (PCC) is a transformative approach in healthcare that prioritizes the individual preferences, needs, and values of patients. We have to learn to treat the person who has a disease and not a disease who has a person. It helps in providing health care and at the same time helps in improving the quality of life.
Person centered care emphasizes on a collaboration between healthcare providers and patients, ensuring that care plans are tailored based on the patient’s own experiences and desires. This approach is not just about treating the illness; it recognizes the patient as a whole person.
Person centered care is not an approach restricted to assisted living facilities, but should also be the approach while we take care of our loved ones in our homes.
Q: That’s a great approach … what does this involve? What are the fundamental elements of person-centered care?
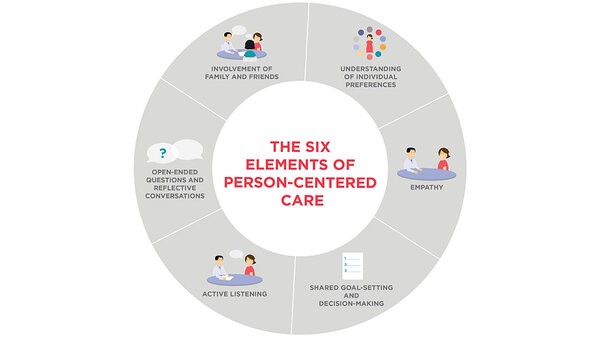
A: The key elements of person-centered care include:
- Respect for Patients’ Preferences – active listening: Healthcare providers should be attentive to the wants and needs of patients. Listen and act accordingly.
- Holistic Approach: Thinking beyond just clinical symptoms to incorporate emotional, social and spiritual health.
- Shared goal setting and decision-making: Patients are active participants in decisions regarding their care.
- Cultural Competence, reflective conversations: Recognizing and respecting diverse backgrounds and lifestyles. Ask open ended questions and have conversations. You can change the approach from time to time.
- Involving Family and friends: sometimes just listening to the person is not enough, speak to members of their family and friends. Ensure that we understand the needs of the person by taking into consideration of opinions from family and friends that matter to the person.
- Empathy: This is key to providing person centered care- put yourself in the person’s shoes and understand that situation. It is not even what I would like if I was in that situation. It’s about what the person needs and you need to understand that each person is unique.

Q: How does person-centered care enhance the care of elderly patients?
A: In elderly care, person-centered care is crucial due to the often-complex health challenges faced by older adults. PCC allows caregivers to consider not just medical conditions but also psychological and social factors. When healthcare is tailored to individual needs, older adults may experience better adherence to treatments and improved health outcomes. This approach fosters a sense of dignity and autonomy, which is important for the overall wellbeing of elderly patients.
By employing PCC principles, healthcare providers can better facilitate the different services that older adults require, such as rehabilitation, mental health support, and social services, ensuring that care is seamless and cohesive.
Q: Since this new facility to serve people with dementia is launched in Goa, how does person-centered care make a difference for individuals with dementia?
A: For patients with dementia, person-centered care can profoundly impact their quality of life. It involves understanding their life story, preferences, and personal history to provide care that respects their identity. PCC strategies — like creating a familiar environment, encouraging communication, and enabling autonomy — can reduce behavioral symptoms and improve overall satisfaction. Instead of a one-size-fits-all approach, tailored interventions honor the individuality of those living with dementia, catering to their unique needs and abilities. It also recognizes the rights of the person and is the right path forward. It’s a different approach and people have to be trained to get this skill.
Q: Why is training in person-centered care essential for healthcare practitioners?
A: Training in person-centered care is paramount because it equips healthcare practitioners with the necessary skills to implement this approach effectively. It encourages empathy, communication and collaboration, which are essential in creating meaningful relationships with patients. It is a skill and one must full understand the principles of person centered care. Moreover, training help providers understand the significance of honoring patients’ voices and facilitating shared decision-making. When practitioners are well-trained in PCC principles, they are more likely to see improvements in patient satisfaction and health outcomes.
Q: What challenges do healthcare professionals face while implementing person-centered care?
A: Implementing person-centered care comes with its challenges. One significant issue is the existing healthcare systems often being structured for efficiency rather than personalization. Time constraints and workload can hinder meaningful interactions between providers and patients. Additionally, there may be a knowledge gap regarding PCC among professionals, leading to inconsistencies in practice. Overcoming these challenges requires systemic changes and a commitment to ongoing education and training in PCC principles.
Q: Finally, what future directions do you envision for person-centered care in healthcare?
A: The future of person-centered care looks promising. As healthcare systems evolve, there is an increasing recognition of the importance of personalized care models. We will likely see a stronger emphasis on integrating PCC with technology, such as using tele-health platforms that allow for more flexible and accessible care. Furthermore, continuing research will help refine PCC practices and demonstrate their efficacy in enhancing health outcomes. The ultimate goal is to create healthcare environments that prioritize the experiences and choices of all patients.