Goa is abuzz with excitement as vintage bike and car owners, users, collectors and fans are decking […]

HMPV is isolated in India, Plan Globally, Act Locally Here is what every citizen needs to know…
Jan 11- Jan 17 2025, MIND & BODY, HEART & SOUL January 10, 2025A Q&A interview with Dr Amit Dias on the HMPV virus
We started the new year of 2025 with the entry of the HMPV virus in India this week. In view of this news going viral, we caught up with Dr Amit Dias from the department of Preventive & Social Medicine at the Goa Medical College to get answers to questions in the minds of the people. Is it going to the next pandemic? Is it the same as COVID-19? How does it spread? What are the symptoms? What do we need to do to stay safe? All this and much more in the information packed here. As the good doctor says, “Emerging and re-emerging infectious diseases are a constant threat. We need to plan globally and act locally.”
Goan Observer: We hear that the HMPV has been detected in India. Where is it currently spreading and what are its implications?
Dr Amit Dias: Yes, this week, India reported its first case of HMPV in an 8- month old boy and 3-month old girl in Bengaluru. Subsequently, more cases have been detected, 2 each in Tamil Nadu and Maharashtra and one in Gujarat. I suspect that there will be many more cases in the country. The detected cases are not linked to China which means the virus is spreading among the people. We need to be alert and not panic. HMPV remains under detected as we do not test for it. The advisory may change based on the newer developments and the health department and NCDC are closely monitoring the situation. The few persons detected with the virus so far are recovering and will be fine.
HMPV has been reported globally, with periodic outbreaks. Recent spikes in cases have been noted in regions of North America, Europe, and Asia. Annual outbreaks occur during late fall, winter and early spring. It is not confined to one geographical area, which underscores its potential for widespread transmission. Prevention is the cornerstone for controlling the spread.
Q: What exactly is HMPV ?
A: HMPV, or Human Metapneumovirus, is a respiratory virus that belongs to the Paramyxoviridae family, closely related to the respiratory syncytial virus (RSV). It primarily affects the respiratory tract, causing illnesses ranging from mild cold-like symptoms to severe respiratory distress, especially in young children, older adults and immune-compromised individuals.
Q: What do we know about the virus?…. is it a new virus?
A: HMPV is not a new virus. It was first isolated in 2001 in the Netherlands and the findings were published in the journal `Nature.’ The team was led by Dr BG Van den Hoogen. They isolated it in 28 children with respiratory infection.
What was also interesting was that retrospective studies (on stored samples) suggest it has been circulating in humans for decades and even found in specimens stored since 1958. Structurally, it is an enveloped RNA virus with a genome prone to mutations, which may affect its transmissibility and severity. We need to keep a close watch on this.
Q: What is the incubation period of HMPV?
A: The incubation period for HMPV ranges from 4 to 6 days. For those who do not understand, incubation period is the time between exposure to the organism to the time of onset of the first symptom. Symptoms usually appear after this period and can persist for 1 to 2 weeks, depending on the individual’s immune response. In China the disease seems to be spreading quickly and mostly affecting children and elderly.
Q: Why do many viruses originate in China? SARS and COVID-19 also originated there.
A: That’s true, several emerging viruses have been identified in China due to its dense population, close human-animal interactions, and thriving wet markets that facilitate zoonotic spillovers. Many of these viruses may occur in animals and they then mutate and gain the ability to jump species and then spread to humans. Some of them could be mild and go unnoticed, while some could be severe like SARS and COVID-19.
However, this phenomenon is not unique to China; similar conditions exist in other parts of the world as well, which have reported emerging infectious diseases.
Q: Do you think HMPV has the potential to become another COVID-19 pandemic?
A: There is no evidence of widespread asymptomatic transmission or rapid mutation leading to new variants. However, continuous monitoring is essential. However, after the COVID pandemic, it would not be wise on our part to take any virus lightly. It is always better to be alert and prevent the pandemic. Though HMPV is a serious respiratory pathogen, it does not currently exhibit the same level of transmissibility or global impact as SARS-CoV-2.
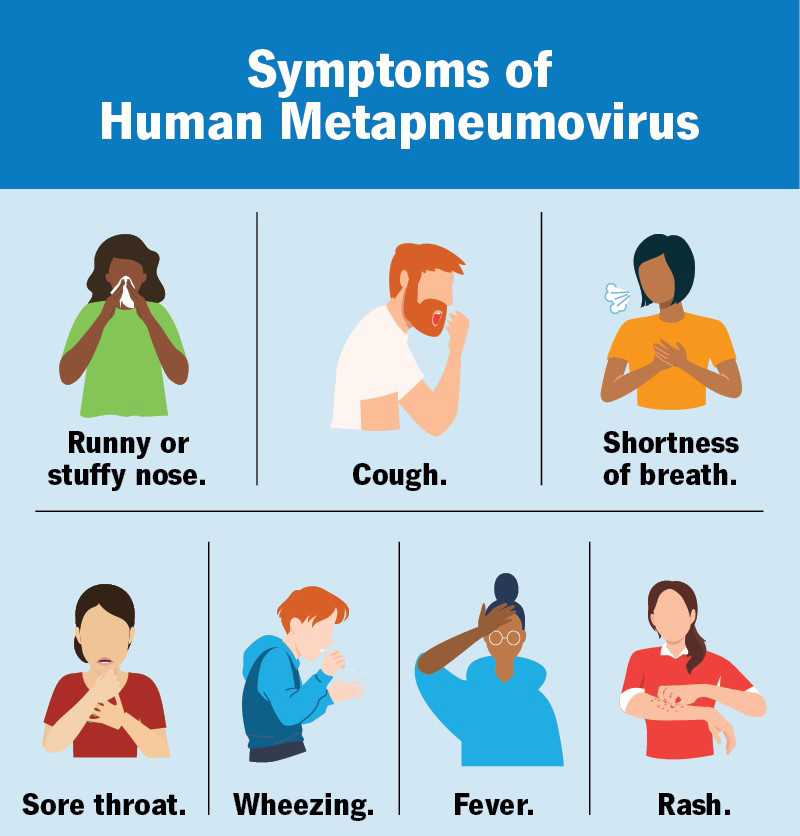
Q: What are the symptoms of HMPV?
A: HMPV could present as influenza like illness (ILI) or severe acute respiratory illness (SARI).
Mild cases will be like a common cold and will have cough, nasal congestion, sore throat and fever.
Severe cases will present with wheezing, shortness of breath, and hypoxia, which may lead to pneumonia or bronchiolitis, especially in vulnerable groups like infants and the elderly.
Q: What can we do to prevent its spread?
A: The prevention strategies are similar to that of COVID-19, except that we do not have a vaccine for HMPV as of now.
Personal hygiene: Regular handwashing and avoiding touching the face.
Respiratory etiquette: Covering the mouth and nose while coughing or sneezing.
Isolation: Staying home when symptomatic to prevent spreading the virus.
Cleaning: Disinfecting surfaces frequently touched by others.
Vaccines: Although no vaccines are available yet, research is ongoing.
Q: What are the do’s and don’ts in case we have an outbreak of HMPV?
A: Do’s and don’ts would be similar to what I explained earlier….
Do’s:
- Cover your mouth and nose with a handkerchief or tissue paper when you cough or sneeze.
- Wash your hands often with soap and water or alcohol-based sanitizer.
- Avoid crowded places and maintain more than an arm’s length from persons affected with the flu.
- Stay away from public places if you have fever, cough, or sneezing.
- Drink plenty of water and eat nutritious food.
- Ensure adequate ventilation with outdoor air in all settings to reduce transmission.
- Stay at home and limit contact with others if you are sick.
- Get enough sleep for proper rest and recovery.
Don’ts:
- Do not shake hands.
- Do not reuse tissue paper or handkerchiefs.
- Avoid close contact with sick people.
- Refrain from frequent touching of your eyes, nose, and mouth.
- Do not spit in public places.
6.Do not take medicines (self-medication) without consulting a physician.
Q: What is the current case fatality rate of HMPV?
A: The exact case fatality is not well-established, but severe cases, particularly in immunocompromised or elderly individuals, can result in higher mortality. Preliminary estimates indicate it is significantly lower than SARS or COVID-19. Mortality rates in elderly range from 10%- 20% in those with severe infections, particularly those with underlying conditions.
Q: How can we prevent HMPV infections in high-risk groups?
A: Same as what I mentioned earlier, besides general preventive measures, high-risk individuals should minimize exposure to crowded places, especially during peak seasons. Enhancing immunity through balanced nutrition, regular exercise, and managing chronic conditions is also beneficial.
Q: Is there any advisory issued by the government?
A: Yes the government is closely monitoring the situation. According to sources, the Chinese officials were also informed to report the development in the country with regards to HMPV so we can be prepared.
The government of India has issued guidelines to enhance preparedness for HMPV, emphasizing timely reporting of Influenza-like Illness (ILI) and Severe Acute Respiratory Infection (SARI) cases on the IHIP portal, alongside proper documentation of lab-confirmed influenza cases. Key measures include isolating suspected cases, following universal precautions to prevent disease spread, and collaborating with private hospitals for accurate reporting and treatment. Authorities must ensure the availability of essential medications, oxygen, and consumables, identify facilities equipped to handle severe cases with ventilator support, and focus on capacity building through hygiene and patient safety training. Awareness among medical and paramedical staff is also prioritized.
Q: What is your message to the readers regarding HMPV?
A: Stay informed, but don’t panic. While HMPV can be severe in certain populations, it is preventable with good hygiene practices and awareness. Let us all play our part in reducing its spread and protecting vulnerable individuals in our communities. Continuous research and surveillance are critical to understanding HMPV’s evolving behavior. Governments and public health organizations must prioritize investments in diagnostic tools and potential vaccine development. Plan globally, act locally.