Goa is abuzz with excitement as vintage bike and car owners, users, collectors and fans are decking […]

SEIZING AWARENESS: A Call To Action On World Epilepsy Day
Feb 15- Feb 21 2025, MIND & BODY, HEART & SOUL February 14, 2025Q&A Interview with Dr Amit Dias
On World Epilepsy Day, we engage in an enlightening discussion with Dr Amit Dias to enhance awareness of epilepsy. As he aptly states, “A seizure can turn your world upside down. Everyone should be aware of epilepsy First AID” In this comprehensive interview he explains the scientific basis of epilepsy, its management, and the latest advancements, including the WHO’s Intersectoral Global Action Plan on Epilepsy and Neurological Disorders (IGAP).
Goan Observer: What is the significance of observing World Epilepsy Day?
Dr Amit Dias: World Epilepsy Day serves as an essential platform for raising public awareness and reducing the stigma associated with epilepsy. A crucial objective is to facilitate the implementation of the World Health Organization’s (WHO) Intersectoral Global Action Plan on Epilepsy and Neurological Disorders (IGAP) (2022-2031). This initiative aims to reinforce a public health approach to epilepsy and achieve global targets that reduce treatment gaps and enhance social inclusion for those affected by the disorder. The day is observed annually on the second Monday of February to encourage collective action toward improving care and support for individuals with epilepsy.
Q: Could you help our readers understand the term epilepsy?
A: The word “epilepsy” has its roots in ancient Greek. It is derived from the Greek word “epilambanein,” which means “to seize” or “to take hold of.” This etymology reflects the condition’s characteristic feature of seizures. Epilepsy is a chronic neurological disorder characterized by recurrent, unprovoked seizures due to excessive, abnormal electrical activity in the brain. These seizures manifest in diverse forms, ranging from brief lapses in awareness to prolonged convulsions. The condition affects individuals of all age groups and can significantly impact quality of life if left untreated.
Q: What exactly constitutes a seizure?
A: A seizure is a transient episode of abnormal neuronal activity in the brain, resulting in various clinical manifestations such as involuntary movements, sensory disturbances, behavioral alterations, or loss of consciousness. During a seizure, the brain experiences sudden, uncontrolled electrical disturbances. The term has been used for centuries to describe this neurological disorder, emphasizing the sudden and often unpredictable nature of seizures experienced by individuals with epilepsy. Seizures may be focal, originating from a specific region of the brain, or generalized, affecting both hemispheres simultaneously.
Q: Is every seizure indicative of epilepsy?
A: No, not all seizures are due to epilepsy. Acute symptomatic seizures can occur as a result of metabolic imbalances, febrile illnesses, head trauma, substance withdrawal, or infections like meningitis. Epilepsy is diagnosed when an individual experiences two or more unprovoked seizures separated by at least 24 hours or has a high probability of recurrence based on medical evaluation.
Q: What are febrile seizures, and how should they be managed?
A: Febrile seizures occur in young children, typically between six months and five years of age, in response to a rapid rise in body temperature. These are usually benign and do not signify epilepsy. If a child experiences a febrile seizure, caregivers should remain calm, position the child on their side to prevent aspiration, remove nearby objects to avoid injury, and attempt to reduce fever using tepid sponging and appropriate antipyretics. It is advisable to seek medical attention to rule out underlying causes and obtain guidance on further management.
Q: What are the predominant causes of epilepsy?
A: Epilepsy can arise from a variety of etiologies, broadly classified into genetic, structural, metabolic, infectious, immune-mediated, and unknown causes. Common risk factors include congenital brain malformations, perinatal injuries, traumatic brain injury, cerebrovascular diseases, central nervous system infections, neurodegenerative disorders, and hereditary predisposition.
Q: Can epilepsy be prevented?
A: While not all cases of epilepsy can be prevented, several measures can mitigate its risk. Preventative strategies include perinatal care to reduce birth-related brain injuries, adherence to traffic safety regulations to prevent traumatic brain injuries, effective management of hypertension and diabetes to reduce stroke-related epilepsy, and timely treatment of neuro infections such as meningitis and encephalitis.
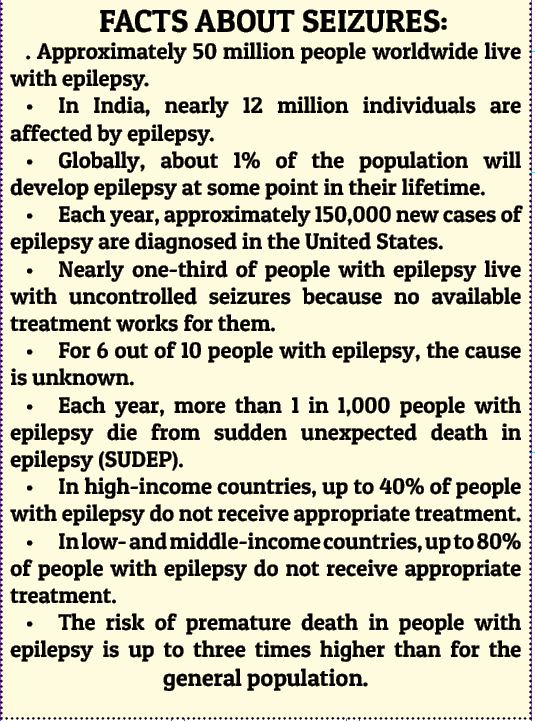
Q: How prevalent is epilepsy globally and in India?
A: Epilepsy is a significant global health concern, affecting approximately 50 million individuals worldwide. India accounts for nearly 12 million cases, making it one of the highest-burden countries. Notably, a substantial proportion of people with epilepsy reside in low- and middle-income regions, where access to specialized care is often limited.
Q: How can seizures be recognized?
A: The clinical presentation of seizures varies widely depending on their type. Common manifestations include:
Tonic-clonic movements: Uncontrollable jerking or stiffness of limbs.
Absence seizures: Brief episodes of staring or unresponsiveness.
Aura or sensory disturbances: Tingling sensations, visual distortions, or olfactory hallucinations.
Behavioral changes: Sudden alterations in mood, confusion, or emotional outbursts.
Loss of postural control: Sudden collapse due to impaired muscle tone.
Autonomic dysfunction: Fluctuations in heart rate, breathing irregularities, or excessive salivation.
It is crucial to recognize that not all seizures involve convulsions, and some may present with subtler symptoms.
Q: What can one do if they see someone getting a seizure?
A: Seizures can appear in different ways, depending on the type. Here’s how to respond to each:
- Generalized Tonic-Clonic Seizure (Grand Mal)
Signs: The person suddenly stiffens, falls, has jerking movements, may lose consciousness, and might drool or have difficulty breathing.
What to Do:
• Stay calm and protect them from injury (move objects away).
• Time the seizure and turn them on their side after jerking stops.
• Do NOT hold them down or put anything in their mouth.
• After the seizure, stay with them until they are fully alert.
Call Emergency Services If:
• The seizure lasts more than 5 minutes.
• Another seizure starts immediately.
• The person is injured, has breathing trouble, or it’s their first seizure. - Absence Seizure (Petit Mal)
Signs: The person stares blankly, stops responding, and may blink or make small repetitive movements. It lasts only a few seconds.
What to Do:
• Gently guide them if they’re in a dangerous place (e.g., crossing a road).
• Do NOT shake or startle them—they will come back on their own.
• Reassure them after the seizure if they seem confused.
Call for help if these episodes happen frequently or if they seem disoriented afterward. - Focal (Partial) Seizure
These can be simple (person remains aware) or complex (person is confused or unaware).
Signs: The person may stare blankly, make unusual movements (lip-smacking, picking at clothes), or walk aimlessly.
What to Do:
• Stay with them and keep them safe.
• If they seem confused, gently guide them away from danger.
• Do not restrain them—let the seizure pass.
• Speak calmly and offer reassurance afterward.
Seek medical help if they don’t return to normal quickly. - Myoclonic Seizure
Signs: Sudden, quick jerks or twitches, usually in both arms or legs. The person remains conscious.
What to Do:
• No immediate first aid is needed.
• If the person falls, help them up and check for injuries.
• Encourage them to see a doctor if seizures become frequent. - Atonic Seizure (“Drop Attack”)
Signs: Sudden loss of muscle control, causing the person to fall suddenly.
What to Do:
• Help them up and check for injuries.
• If it’s their first seizure, advise them to seek medical help.
• Some people wear helmets to protect against head injuries from falls.
What to Do After a Seizure (Post-Seizure Care)
• Stay with the person and speak calmly.
• They may be confused, tired, or need to rest.
• Explain what happened if they don’t remember.
• If they’re injured, get medical help.
• Do NOT give food, drink, or medicine until they are fully awake.
Q: What is your key message for World Epilepsy Day?
A: World Epilepsy Day is a vital occasion to advocate for improved epilepsy care, enhance public awareness, and combat stigma. It is imperative to bridge knowledge gaps, promote early diagnosis and treatment, and foster an inclusive society for individuals with epilepsy.
The implementation of the WHO IGAP framework offers a promising pathway toward achieving these goals. Let us collectively work towards a world where epilepsy is understood, treated effectively, and no longer a cause for discrimination.